The main cause of acute coronary syndrome (ACS) is a blockage or obstruction in coronary arteries. This blockage is commonly caused by a cholesterol-rich plaque, often referred to as a thrombus. A plaque may show abnormalities in heart activity on the electrocardiogram. Common symptoms of ACS may manifest as shortness of breath or chest pain.
Introduction
ACS is a significant health concern due to the morbidity and mortality associated with it. Physicians may consider a patient’s cardiac biomarkers, electrocardiography findings, and the history and symptoms of a patient. The primary goal of treatment is to rapidly restore blood flow surrounding arterial blocks (rapid reperfusion) and treat the narrowing of coronary arteries (primary percutaneous coronary intervention).
In terms of preventive strategies, professional guidelines by the American College of Cardiology (ACC) and American Heart Association (AHA) uphold decreasing risk factors including diabetes mellitus, hypercholesterolemia, hypertension, and smoking.
Aspirin is generally the first line of treatment. Recommended therapies include dual antiplatelet therapy, and the use of anticoagulants, beta-blockers, angiotensin receptor blockers, and angiotensin-enzyme converting inhibitors. Reperfusion therapy may be administered in eligible cases. Common Symptoms of Acute Coronary Syndrome.
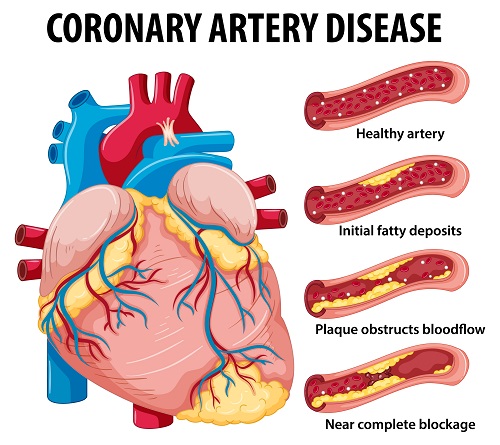
Coronary Artery Disease for health education Infographic illustration
To confirm a diagnosis of acute coronary syndrome, your physician may check the presence of obvious symptoms:
- Pain in the arm, jaw, or stomach
- Pain experienced at rest or with exertion
- Shortness of breath, especially when exercising
- Pressure in the chest
- Sweating
Pharmacological Approaches for Acute Coronary Syndrome
- The antithrombotic drug aspirin is one of the most effective, and inexpensive therapies for acute coronary syndrome (antithrombotics help reduce blood clot formation).
- Heparin is the most widely used anticoagulant for acute coronary syndrome (anticoagulants make blood thinner to increase clotting time).
- Thrombolytics or clot busters help remove an artery-blocking blood clot.
- Nitroglycerine may be used for momentarily widening blood vessels and increasing blood flow.
- Antiplatelet medications such as aspirin, clopidogrel (Plavix), prasugrel (Effient), and others help stop the formation of blood clots.
- Beta-blockers help relax the muscles in your heart and slow down your heart rate. They reduce the demand for your heart and lower your blood pressure. In this case, metoprolol (Lopressor, Toprol-XL) and nadolol (Corgard) may be used.
- Inhibitors of the angiotensin-converting enzyme (ACE) expand blood vessels and increase blood flow, helping the heart to function better. This category of medication may include Lisinopril (Prinivil, Zestril), Benazepril (Lotensin), and others.
- Like irbesartan (Avapro), losartan (Cozaar), and angiotensin receptor blockers (ARBs) help regulate blood pressure.
- Statins decrease the amount of blood cholesterol, making more stable plaques that do not rupture easily. Atorvastatin (Lipitor), Simvastatin (Zocor, Flolipid) are common statins used in ACS therapy. Medical Procedures Involved
Several diagnostic tests are associated with ACS. You may be asked to undergo one or more tests from the list indicated below:
- Blood tests may be prescribed to detect enzymes that may be secreted as a result of cell death or damage to the heart tissue. When blood tests show a positive result, you may have a higher likelihood of experiencing a heart attack.
- Coronary angiogram uses X-ray imaging to view the blood vessels of your heart. The test is carried out by inserting a catheter through the artery in your arm, all the way to the cardiac arteries. A dye is inserted that flows through the arteries and its movement is recorded using X-rays. The test reveals narrow or blocked arteries.
- Electrocardiogram (ECG) is a procedure in which electrodes are attached to the skin to measure electrical impulses. Irregular impulses may refer to a dysfunction or a heart deficient in oxygen. An ECG may also reveal a blockage in terms of the patterns of impulses.
- Myocardial perfusion imaging reveals blood flow through heart muscle. A radioactive substance injected in the blood reveals patterns of blood flow including the quantity of blood flowing and the areas of reduced blood flow.
- Echocardiogram uses sound waves directed to the heart to produce a “live image” of the heart. This procedure detects whether the heart is pumping properly.
- Stress tests show the condition of the heart during exercise or through medication that deliberately increases the heart rate. Stress tests are usually administered to patients who do not show signs of ACS or other conditions that may be life-threatening. The state of the heart is usually visible through the use of an echocardiogram, ECG, or myocardial perfusion imaging during the stress test.
- Computerized tomography angiogram uses a number of images displaying 2D cross-sections of the heart. The purpose of this form of imaging is to detect coronary arteries that have been narrowed or blocked.
Surgical Interventions Your doctor may recommend one of the following procedures to restore blood flow to your heart muscles:
- Angioplasty and stenting procedures – During this surgery, the doctor inserts a catheter or long and thin tube into the blocked or narrowed portion of your artery. A wire with a deflated balloon is conveyed to the narrowed region via the catheter. By compressing the plaque deposits against your artery walls, the balloon is then inflated, expanding the artery. There is normally a mesh tube (stent) left in the artery to help hold the artery intact.
- Surgery for coronary bypass – A surgeon takes a piece of the blood vessel (graft) from another part of the body and establishes a new blood path that goes through (bypasses) a blocked coronary artery.
Effects of the COVID-19 Pandemic on Acute Cardiology Care
Inpatient treatment and bed redistribution has undergone a massive shift, with many wards converted into units for handling COVID-19 situations. COVID-19 has been a major influence, especially on inpatient cardiology and the length of stay of acute cardiology patients. ICUs, being occupied by critical COVID-19 cases can no longer accommodate cardiothoracic surgery patients or acute cardiology patients.
COVID-19 also tends to increase the number of false positives related to ACS as the condition may present ECG changes and clinical myopericarditis syndrome mimicking ACS. 18% – 23% COVID-19 patients exhibit troponin elevation, even in the absence of chest pain. About 7% of COVID-19 deaths may be traced to fulminant myocarditis. Fulminant myocarditis (FM) is a fatal cardiac condition that results due to a rapid decline in cardiac function. FM may be diagnosed using a number of techniques including echocardiography, cardiac magnetic resonance, and others.
A drop in ACS cases post-pandemic may not necessarily be true as it may reflect the reluctance of patients to attend the hospital. Another important impact of the COVID-19 crisis is on the healthcare workers offering cardiology services, more so those related to aerosol-generating procedures, or the ones involved in ambulance transport, echocardiography, and urgent percutaneous procedures. How KareOptions Can Help if you are Dealing with ACS
KareOptions is the right destination for seeking an optimal diagnosis and treatment plan. Given the inherent complexities involved in dealing with ACS, KareOptions focuses on a second opinion as your best route to a convincing plan of recovery. Our Medical Second Opinion Service (MSOS) and Second Opinion Board Review (SOBR) focuses on offering the best specialists in cardiac care to help you understand your possible options and support you through your treatment journey. We also offer end-to-end care coordination through our Continuity of Care (COC) and Transfer of Care Coordination (TOCC) services.
Disclaimer:
“KareOptions does not have any intention to provide specific medical advice, but rather to provide its users and/ or the general public with information to better understand their health. All content (including text, graphics, images, information, etc.) provided herein is for general informational purposes only and is not a substitute for professional medical advice, care, diagnosis, or treatment. KareOptions makes no representation and assumes no responsibility/ liability for the accuracy of the information, advice, diagnosis, treatment provided herein or on its website. NEVER DISREGARD PROFESSIONAL MEDICAL ADVICE OR DELAY IN SEEKING TREATMENT BECAUSE OF SOMETHING YOU HAVE READ IT HERE OR ACCESSED THROUGH THE KAREOPTIONS WEBSITE.


