What is Cervical Cancer?
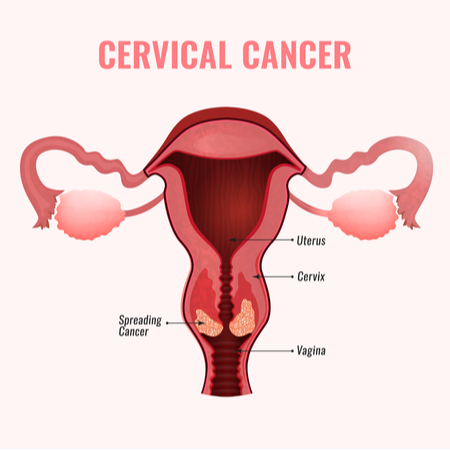
Cervical cancer is a type of cancer that occurs in the cells of the cervix — the lower part of the uterus that connects to the vagina. Cervical cancer happens when cells change in a women’s cervix. Cancer starts when cells in the body begin to grow uncontrollably. It has been found that cervical cancer can affect the deepest tissues of the cervix and has the possibility of spreading to other parts of the body, like the lungs, liver, bladder, vagina, and rectum. The cervix comprises two parts and is also covered with two varied types of cells. The endocervix” also known as the cervical canal is the opening of the cervix. This opening leads into the uterus. It is covered with glandular cells. The exocervix is also known as ectocervix is the portion of the uterus. This portion extends into the vagina. It is the outer part of the cervix that can be seen by the doctor during a speculum exam. It is covered in squamous cells. T-Zone- The area where these cells meet is called the “transformation zone” (T-zone) and is the most likely location for abnormal or precancerous cells to develop.
Pre-cancers of the cervix: Abnormal changes which are also termed pre-cancerous, slowly take place in the normal cells of the cervix first, leading to a gradual change in the cells present in the transformation zone which causes the development of cancer. There are several terms that specialists use to describe these precancerous changes, cervical intraepithelial neoplasia (CIN), squamous intraepithelial lesion (SIL), and dysplasia. These pre-cancers are then graded in the lab on a scale of 1 to 3 based on how much of the cervical tissue looks abnormal.
Least serious Cervical pre-cancer: In CIN1 (also called mild dysplasia or low-grade SIL), not much of the tissue looks abnormal, and that is why it is considered as the least serious cervical pre-cancer. • Most serious pre-cancer- In CIN2 or CIN3 (also called moderate/severe dysplasia or high-grade SIL) more of the tissue looks abnormal that is why high-grade SIL is the most serious type of pre-cancer. It is very crucial to treat cervical pre-cancers to prevent almost all types of cervical cancers, as cervical cancers originate from the cells undergoing pre-cancerous changes, while some women with pre-cancerous cells will develop cancer, for most women pre-cancerous cells will vanish without any treatment. Hence such cases need immediate attention where pre-cancers turn into cancers.
Types of Cervical Cancer
Every cervical cancer patient is different. The classification of Cervical cancer is based on their appearance in the labs when viewed under a microscopic lens. Once the type of your cervical cancer has been established, determining the prognosis and treatment plan becomes easier. There is more than one kind of cervical cancer. The main types of cervical cancer are:
- Squamous cell carcinoma- This type of cervical cancer gets initiated in the thin, flat cells also known as squamous cells, lining the outer part of the cervix, which projects into the vagina. Most cervical cancers are known to be squamous cell carcinomas. It is found in up to 90% of cases. Squamous cell carcinomas most often begin in the transformation zone (where the exocervix joins the endocervix).
- Adenocarcinoma- This type of cervical cancer begins in the column-shaped glandular cells that line the cervical canal. Cervical adenocarcinoma develops from the mucus-producing gland cells of the endocervix. The treatment plan for Adenocarcinoma is like the treatment plan for squamous cell cancer of the cervix.
- Mixed Carcinoma- This has features of both squamous cell carcinomas and adenocarcinomas. Sometimes, both types of cells are involved in cervical cancer. Very rarely, cancer occurs in other cells in the cervix. This is a rare type of cervical cancer.
Majorly all cervical cancers can be classified as either squamous cell carcinomas or adenocarcinomas, other types of cancer also can develop in the cervix. Sarcoma, melanoma, and lymphoma are a few other types of cancers that occur more commonly in other parts of the body.
Causes of Cervical Cancer
Cervical cancer gets triggered when healthy cells present in the cervix develop changes or mutations in their DNA. It gets initiated in the tissue because of unusual changes. DNA of the cell carries instructions that tell a cell what to do. Studies share that healthy cells grow and multiply at a set rate, eventually dying at a set time whereas the mutations tell the cells to grow and multiply out of control, because of which they do not die. This in turn leads to the accumulation of abnormal cells forming a mass (tumor). Cancer cells invade nearby tissues and can break off from a tumor to spread (metastasize) elsewhere in the body.
Human papillomavirus (HPV) infection is the major risk factor for cervical cancer. Human papillomavirus or HPV is the main cause of cervical cancer. Most cases are caused by infection with this virus only and are preventable with a vaccine. HPV has got multiple strains, a sexually transmitted infection, play a role in causing most cervical cancer. The body’s immune system typically prevents the virus from doing harm when exposed to HPV, so there’s usually time to find and treat it before it causes serious problems. In a small percentage of people, however, the virus survives for years, contributing to the process that causes some cervical cells to become cancer cells.
More than 100 types of HPV have been found to exist. Some are likely to cause more complications than others. These HPV’s are further categorized as low-risk and high-risk HPV. It has been noticed that low-risk types cannot cause cervical cancer and are usually treatable. Whereas high-risk types of HPV can cause abnormal cells formation on the cervix, which can develop into cancer if they are left untreated.
Let us understand the most common types of HPV. Identifying the type of HPV contracted by you, helps your doctor determine the next steps. Some types of HPV clear up without intervention. Other types may lead to cancer. Here the role of the doctor is very important in monitoring your condition so that if cancer cells do develop, they can be detected early. Listed below are the types of HPV:
Low-risk category: HPV 6 and HPV 11 fall into the low-risk category of HPV. HPV 11 can also cause changes to the cervix and is known to cause genital warts. Genital warts look like cauliflower-shaped bumps on your genitalia. They usually appear a few weeks or months after exposure from a sexual partner who has HPV. Getting vaccinated by HPV vaccine may help prevent HPV 6. The vaccine has also been found to offer some protection from HPV 11.
High-risk category: The most common and high-risk type of HPV is HPV 16. It usually doesn’t result in any major symptoms, even though it can bring about cervical changes. It has been found to causes 50 % of cervical cancers worldwide. Another high-risk type of HPV is HPV 18. It is generally not found to cause any symptoms, but it can lead to cervical cancer. HPV 16 and HPV 18 are together responsible for approximately 70 percent of all cervical cancers worldwide.
Women between the age group of 35 to 44 years old are most likely to get it. More than 15% of new cases are in women above the age group of 65 years, especially those who have not been getting regular screenings.
The risk of developing cervical cancer can be reduced by having regular screening tests and receiving a vaccine that protects against HPV infection.
A recent Large Study Confirms that HPV Vaccine Prevents Cervical Cancer. In the study of nearly 1.7 million women, the vaccine’s efficacy was particularly pronounced among girls vaccinated before age 17, among whom there was a nearly 90% reduction in cervical cancer incidence during the 11-year study period (2006 through 2017) compared with the incidence in women who had not been vaccinated. Being infected with a cancer-causing strain of HPV does not necessarily mean that you will get cervical cancer. Our body’s immune system is effective in washing out most HPV infections, often within a span of two years. HPV is also known to cause other cancers in women and men. These include vaginal cancer, vulvar cancer, penile cancer, anal cancer, rectal cancer, and throat cancer.
Symptoms of cervical cancer
Cervical cancer at the very early stage usually does not showcase any signs or symptoms hence, many times women with cervical cancer do not realize they have the disease. When symptoms do appear, they are easily mistaken for common conditions like menstrual periods and urinary tract infections (UTIs). Let us understand the signs and symptoms of more-advanced cervical cancer which include:
• Unusual vaginal bleeding after intercourse,
• Bleeding between periods or after menopause
• Watery and sometimes bloody vaginal discharge that may be heavy and have a foul odor
• Pelvic pain or pain during intercourse • Needing to urinate more often
• Pain during urination
Stages of cervical cancer
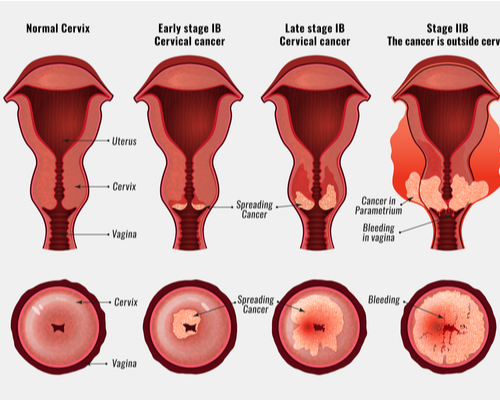
Working out the stage of cancer is important, as it helps a person decide the most effective type of treatment. Stage describes the degree of your cancer cells, such as just how large the growth is, as well as if it has spread out. Staging also assesses whether cancer has reached nearby structures or more distant organs. After you have been diagnosed, your doctor will assign your cancer a stage. Knowing the stage of your cancer can help your physician find the right treatment for you.
A 4-stage system is the most common way to stage cervical cancer.
- Stage 0: Precancerous cells are present.
- Stage 1: At this stage, the cancer is small. Cancer cells have grown from the surface into deeper tissues of the cervix, and possibly penetrated the uterus and to the nearby lymph nodes.
- Stage 2: At stage 2 cancer is found to grow beyond the cervix and uterus, but not as far as the walls of the pelvis or the lower part of the vagina. There is a possibility that it may or may not affect nearby lymph nodes.
- Stage 3: This stage sees the penetration of the cancer cells to the lowest part of the vagina or the walls of the pelvis, and it might act as a blockage point for the ureters, the tubes that carry urine from the bladder. It may or may not affect nearby lymph nodes.
- Stage 4: At this stage cancer starts affecting the bladder or rectum and is observed to be growing out of the pelvis. It may or may not affect the lymph nodes. Later in stage 4, it will spread to distant organs, including the liver, bones, lungs, and lymph nodes.
It is very important to note here that undergoing screening and seeking medical attention if any symptoms occur can help a person positively by getting access to early treatment thereby increasing the chances of life expectancy and survival.
Related Blogs
Cervical Cancer Screening- What every Woman can do to prevent #CervicalCancer?
References: https://www.cancerresearchuk.org/about-cancer/cervical-cancer/stages-types-grades/types-and-grades https://www.cancer.org/cancer/cervical-cancer/about/what-is-cervical-cancer.html https://www.webmd.com/cancer/cervical-cancer/cervical-cancer#1
https://www.mayoclinic.org/diseases-conditions/cervical-cancer/symptoms-causes/syc-20352501 https://www.healthline.com/health/cervical-cancer#causes
https://www.medicalnewstoday.com/articles/159821#stages
https://www.everydayhealth.com/cervical-cancer/prevention.aspx
https://www.cancer.gov/types/cervical/patient/cervical-screening-pdq https://www.cdc.gov/cancer/cervical/basic_info/screening.htm https://nutritionguide.pcrm.org/nutritionguide/view/Nutrition_Guide_for_Clinicians/1342026/all/Cervical_Cancer https://www.everydayhealth.com/cervical-cancer/prevention.aspx
https://www.roswellpark.org/cancertalk/202001/can-you-have-kids-after-cervical-cancer
Disclaimer
KareOptions does not have any intention to provide specific medical advice, but rather to provide its users and/ or the general public with information to better understand their health. All content (including text, graphics, images, information, etc.) provided herein is for general informational purposes only and is not a substitute for professional medical advice, care, diagnosis, or treatment. KareOptions makes no representation and assumes no responsibility/ liability for the accuracy of the information, advice, diagnosis, treatment provided herein or on its website. NEVER DISREGARD PROFESSIONAL MEDICAL ADVICE OR DELAY IN SEEKING TREATMENT BECAUSE OF SOMETHING YOU HAVE READ IT HERE OR ACCESSED THROUGH THE KAREOPTIONS WEBSITE.”